Cancer pain
Although pain is one of the most common symptoms of cancer, many people with cancer do not receive effective pain relief. You might think that the pain (which may be caused by the cancer itself,1,2 infection,1 or the cancer treatment2) is something that you just “have to put up with”, but that is most definitely not the case.2 If you are in pain at any stage during the cancer journey, then do tell your doctor or nurse and ask them what can be done to help.
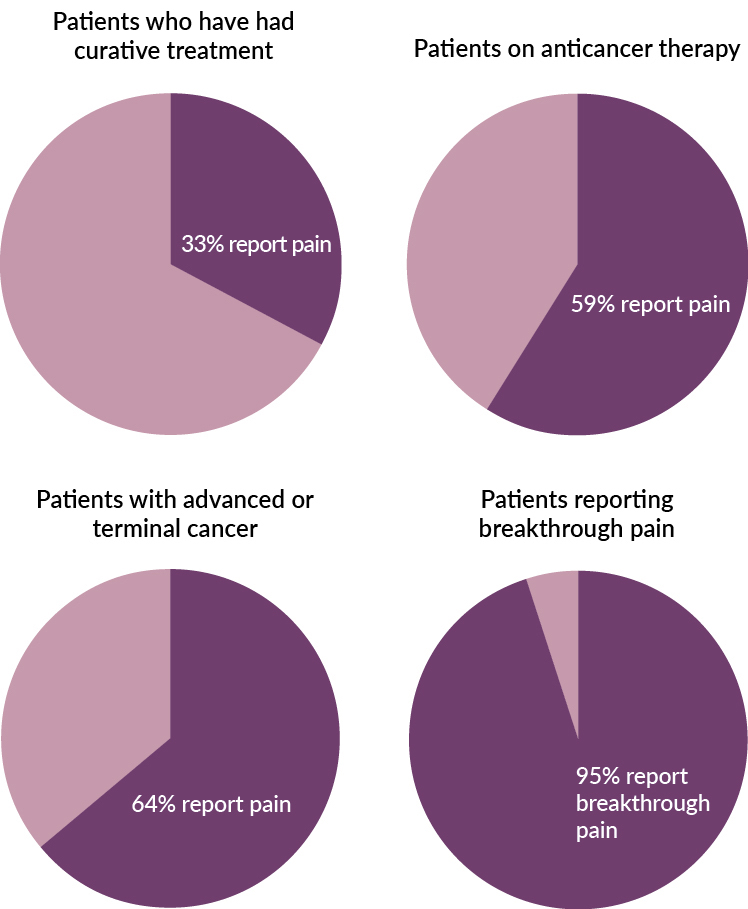
Pain prevalence in people with cancer
Treating cancer pain
Your doctor or nurse, or another member of your care team, might suggest one of the methods from the following list to help to control your pain. Sometimes a combination of methods might be the most helpful.
- Medication: your doctor may suggest painkilling medication, either a medication that can be bought from the chemist or supermarket or a stronger medication that is only available on prescription. Some painkilling medications can be swallowed, while others have to be given as an injection4
- Cancer treatments: treatments such as chemotherapy and radiotherapy may reduce the pain by shrinking your tumour; this eases the pain by decreasing the pressure the tumour exerts on surrounding tissue and nerves4
- Specialised techniques: there are a number of specialised techniques that may be used to control pain when classical treatments do not work; these include the following, but your doctor may be able to suggest others that are not on this list:
- Strengthening bones: procedures using cement to strengthen weak bones may be help reduce bone pain4
- Debulking surgery: removes the tumour, or reduces the size of the tumour, which decreases the pressure it exerts on surrounding tissue and nerves4
- Neuromodulation: a procedure that alters nerve activity using electrodes or chemicals4
- Complementary therapies: some non-traditional, or “alternative”, therapies may also be useful; these therapies could include massage, meditation, acupuncture, or cognitive behavioural therapy (CBT)5
- Self-help: simple strategies such as listening to calming music or breathing slowly and deeply can help you relax so that the pain does not seem as bad4
- Counselling: talking to a counsellor may help relieve stress and tension and make it easier to cope with pain4
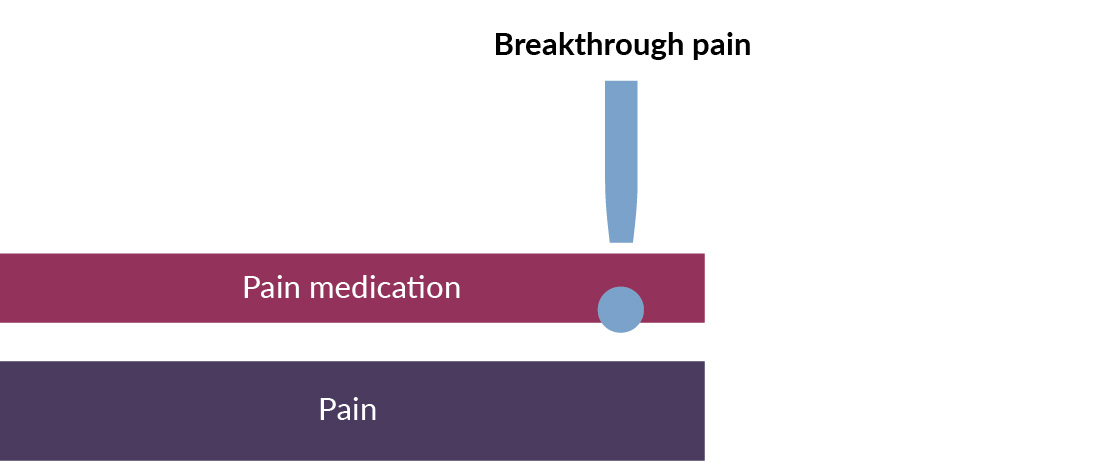
Breakthrough pain
Even if you are currently receiving treatment for pain, you may experience a flare-up of pain, called “breakthrough pain”. Breakthrough pain is a sudden burst of pain that you feel even though your other pain is well controlled. Breakthrough pain is severe and comes on suddenly, usually reaching a peak within 5 minutes. Breakthrough pain episodes do not usually last longer than 30 to 60 minutes, and do not occur more than four times a day.1
Breakthrough pain episodes can be further classified as “spontaneous” or “incident”.
- Spontaneous pain is unpredictable; it comes out of the blue and is not related to any specific activity
- Incident pain is linked to a specific event or trigger such as moving or coughing; it can be predictable, e.g. it may always happen when you are having your wound dressed1
This type of pain can be very upsetting. It can seriously affect your general well-being and can affect your ability to carry out daily tasks. It can also make you feel depressed and/or anxious, and reduce your quality of life.1,6 It can make you feel very uncertain and raise all kinds of spiritual doubts, even if you are not religious; these complicated feelings can be difficult to process and even make the pain worse.6
If you think you are experiencing breakthrough pain, it is very important to ask your doctor or nurse to suggest ways to manage the pain.
Treating breakthrough pain
Breakthrough pain can be managed in a number of different ways. Different members of your care team may be involved, and you may be treated using one or a combination of the following methods.1
- Medication: it may help if your doctor prescribes an extra or new medication or adjusts your current pain treatment. A typical treatment is to continue with the painkilling medication that you are already receiving, with the addition of an extra medication to be used as soon as the breakthrough pain starts1
- Preventing predictable triggers: if you know when the breakthrough pain is likely to occur, or if you know what sets it off, then it might be possible to avoid it. For instance, if you know that breakthrough pain is triggered by coughing, your doctor may prescribe cough medication so that you do not cough1
- Targeting underlying cause of pain: treating the underlying cause of the pain (e.g. cancer or infection), rather than the pain itself, can also be an option1
- Lifestyle changes: changing your lifestyle may help reduce pain; for instance, if you know that the pain is worse when you are tired, then it may help to take regular breaks or to ask your family to help with tiring activities; specific exercises may also help relieve pain1
- Complementary therapy: some non-traditional, or “alternative” therapies may also be useful in the treatment of breakthrough pain; these therapies could include massage, meditation, acupuncture, and CBT1
- Intervention techniques: some specialised methods such as neuroablation or neuromodulation may be useful. If other methods have not helped relieve the breakthrough pain you are experiencing, your doctor may suggest one of these methods to you, and will explain what it involves1
Recording your pain
It may be useful to keep a logbook about the pain you are experiencing, by writing the following in a notebook or on your phone or tablet.
- Record the date and time you experience the pain, and how long it continues2,3
- In which part of your body does the pain occur? Does it stay in that one spot or does it spread?2
- What activities cause the pain (e.g. a particular movement or sitting or lying still),3 and when does the pain start?2,3
- What does the pain feel like (e.g. aching, throbbing, stabbing, cramping)?2,3
- Does your pain interfere with your daily activities such as work or caring for your family?1,2
- Rate the pain on a scale of 1 to 10 (1 = no pain; 10 = worst possible pain), and note what makes the pain better or worse2,3
- Take your logbook to your next doctor’s appointment
Glossary